Gallstones, the small, pebble-like deposits that form in the gallbladder, are more than just a medical curiosity. For many, they are a source of intense pain and discomfort. Although they might seem insignificant due to their size, gallstones can lead to severe complications if left untreated.
Every year, a substantial number of people experience symptoms that prompt a visit to the doctor, only to discover that they have these little intruders lurking in their gallbladder.
Understanding the treatments available for gallstones is crucial, not just for those diagnosed with the condition, but also for individuals who want to be informed about potential health challenges they or their loved ones might face in the future.
In this article, we will delve into the three primary treatments for gallstones, giving you a comprehensive look at the options available and helping you understand what to expect from each.
Whether you’re on a journey to manage your own gallstones or are merely curious, read on to empower yourself with knowledge on this prevalent health topic.
Understanding Gallstones
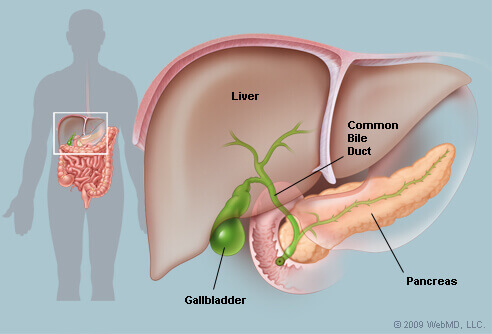
Gallstones are hardened deposits that form within the gallbladder, a small, pear-shaped organ located beneath the liver. These stones can vary in size from as tiny as a grain of sand to as large as a golf ball. While some people may have a single large stone, others might have many smaller ones. Let’s break down the basics of gallstones and understand their types.
Types of Gallstones
1. Cholesterol Stones
- These are the most common type of gallstones, accounting for about 80% of all gallstones.
- They are usually yellow-green in color.
- Despite the name, they aren’t just made of cholesterol but are often a mix of cholesterol, bilirubin, and other substances.
Recommended: What Antibiotics Treat Gallbladder Infections?
2. Pigment Stones
- These stones are darker and are formed when there’s an excess of bilirubin in the bile, a fluid produced by the liver that helps in the digestion of fat.
- They can be black or brown.
- Black pigment stones generally arise due to conditions that cause increased bilirubin production, like cirrhosis or certain blood disorders.
- Brown pigment stones can result from infections, prolonged bile duct obstruction, or certain inherited conditions.
Common Symptoms and Complications
While many people with gallstones won’t experience any symptoms (known as “silent” gallstones), others might experience intense bouts of pain called gallstone attacks. These attacks can last from a few minutes to several hours.
Common symptoms include:
- Sharp pain in the upper abdomen, which might radiate to the right shoulder or back.
- Nausea or vomiting.
- Fever or chills.
- Jaundice (yellowing of the skin and eyes).
- Dark urine and clay-colored stools.
Potential Complications:
- Inflammation of the Gallbladder (Cholecystitis): Persistent gallstones can lead to inflammation, causing severe pain and fever.
- Blockage of the Common Bile Duct: Gallstones can migrate to the common bile duct, leading to jaundice and bile duct infection.
- Blockage of the Pancreatic Duct: This can result in pancreatitis, an inflammatory condition of the pancreas.
- Gallbladder Cancer: Rarely, longstanding untreated gallstones might increase the risk of gallbladder cancer.
Recommended: Can Gallbladder Symptoms Go Away?
Understanding the nature, symptoms, and potential complications of gallstones can guide decisions regarding the necessity and urgency of treatment. Whether through observation or intervention, the goal is to prevent complications and alleviate symptoms.
Factors Influencing Treatment Choice
When it comes to gallstones, there isn’t a one-size-fits-all approach to treatment. The best course of action depends on several factors related to the individual’s health status, the nature of the gallstones, and the potential risks associated with each treatment method. Here’s a closer look at these influencing factors:
1. Size and Type of Gallstones
- Cholesterol Stones: Since these stones often form due to an imbalance of substances that make up bile, certain treatments, like oral dissolution therapy, may be effective in dissolving them.
- Pigment Stones: These might be harder to treat with non-surgical interventions, especially if they are large or numerous.
- The size of the gallstones plays a role too. Small stones might pass on their own or may be suitable for less invasive treatments, while larger stones might necessitate surgical intervention.
2. Symptom Presence
- Silent Gallstones: Not all gallstones cause symptoms. If they don’t, and there’s no risk of complications, doctors might recommend a watchful waiting approach.
- Symptomatic Gallstones: If gallstones cause pain or other symptoms, treatment might become necessary. The intensity and frequency of these symptoms can influence the urgency of the treatment.
3. Patient’s Overall Health and Other Existing Medical Conditions:
- Age, overall health status, and co-existing medical conditions can influence the treatment approach. For instance:
- Patients with diabetes might be at a higher risk of infections, which can influence the decision to perform surgery.
- Individuals with other digestive system disorders might require special consideration when determining the best treatment.
- Certain conditions might increase the risk of complications from gallstones, pushing toward more aggressive treatment.
4. Potential Risks of Treatment
- Each treatment comes with its own set of risks. Evaluating these risks against the potential benefits is essential.
- For example, while surgery might offer a permanent solution, it carries surgical risks like infections, bleeding, and reactions to anesthesia.
5. Patient Preference
- Some patients might prefer to try non-surgical interventions before considering surgery, even if the chances of success are limited.
- Others might opt for surgery immediately to reduce the risk of recurrent symptoms or potential complications.
Recommended: Does Gallbladder Hurt More In The Morning?
6. Professional Medical Opinion
By considering the above factors, healthcare professionals and patients can collaboratively decide on a treatment strategy that aligns with the patient’s needs and the medical circumstances surrounding the gallstones.

What Are The 3 Treatments For Gallstones?
Treatment 1: Nonsurgical Treatments
Nonsurgical treatments are often the first line of approach, especially for patients who may not be ideal candidates for surgery or for those who prefer less invasive solutions. While these treatments might not be suitable for all, they can offer relief for many. Let’s delve deeper into the nonsurgical options available for treating gallstones:
1. Observation and Symptomatic Treatment
For individuals with silent gallstones (those that do not cause symptoms), the initial approach is often observation. The idea here is to monitor rather than intervene, given that not all gallstones lead to complications.
Pain Management: If occasional pain does occur, over-the-counter pain relievers such as acetaminophen or ibuprofen can be used. However, it’s crucial to consult with a healthcare provider to ensure these are safe and effective.
Dietary Recommendations: Eating a balanced diet and avoiding fatty foods can sometimes help manage symptoms. Meals high in fiber and low in saturated fats can promote gallbladder health.
2. Oral Dissolution Therapy
This therapy involves taking medications orally to dissolve gallstones. It’s more effective for cholesterol stones than for pigment stones.
Medications: The primary medications used for this purpose are bile acids, specifically ursodiol (Actigall, Urso) and chenodiol (Chenix). They work by thinning the bile, allowing cholesterol stones to dissolve gradually.
Duration and Effectiveness: The treatment can take months or even years to be effective, and there’s a risk of gallstones reforming if therapy is discontinued. The success rate is variable, with smaller stones (less than 1.5cm in diameter) generally dissolving better than larger ones.
Side Effects: These medications are generally safe but can sometimes cause minor side effects such as diarrhea. Moreover, they are not suitable for everyone, especially those with a non-functioning or infected gallbladder.
3. Contact Dissolution Therapy
This is a less common method where a drug is directly injected into the gallbladder to dissolve stones. It’s still experimental and not widely available.
Procedure: Under imaging guidance, a catheter is inserted into the gallbladder, and a solvent (like methyl tert-butyl ether) is introduced to dissolve the stone.
Duration and Effectiveness: It can dissolve cholesterol gallstones within hours, but due to potential risks and its experimental nature, it’s reserved for specific situations where other methods are not feasible.
Side Effects: There’s potential for toxicity and complications, and as such, it’s not the first line of treatment.
Recommended: Can Gallstones Wake You Up?
It’s important to note that while nonsurgical treatments can be effective for certain individuals, they might not provide a permanent solution. Gallstones can recur, especially after stopping oral dissolution therapy. Hence, patients opting for these treatments should be under regular medical supervision to monitor any changes or potential complications.
Treatment 2: Minimally Invasive Procedures
Minimally invasive procedures have revolutionized the way many medical conditions, including gallstones, are treated. By minimizing large incisions and the trauma associated with open surgeries, these procedures often result in quicker recovery times, reduced hospital stays, and less post-operative pain.
Here’s an in-depth look into the minimally invasive methods used for gallstones:
1. Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is a specialized procedure primarily used to treat gallstones that have migrated out of the gallbladder and into the bile duct, where they can cause blockages.
Procedure: A flexible, lighted tube (endoscope) is inserted through the mouth, down the esophagus, and into the stomach and the first part of the small intestine. A dye is injected into the bile ducts through the endoscope, which allows them to be seen on an X-ray. Special tools can then be used to open the bile duct entrance and remove or crush the stone.
Benefits: Directly addresses and removes the problematic stone(s) causing a blockage. Can prevent or treat jaundice, pancreatitis, or cholangitis (bile duct infection) caused by the blocked ducts.
Risks: Like all procedures, ERCP carries some risks, such as pancreatitis, infections, bleeding, or perforation.
2. Gallbladder Drainage (Percutaneous Cholecystostomy)
This procedure might be considered for patients with an inflamed gallbladder (acute cholecystitis) who are not immediate candidates for surgery due to high risk.
Procedure: Under imaging guidance, a thin needle is inserted through the skin directly into the gallbladder. A catheter is then placed, allowing the gallbladder to drain its contents, thus alleviating the inflammation.
Benefits: Provides temporary relief from symptoms of acute cholecystitis. Can stabilize a patient’s condition before potential surgery.
Risks: Possible complications include bile leakage, infections, or injury to surrounding structures.
3. Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL is a procedure that uses shock waves to break up stones in the gallbladder, making them small enough to pass through the bile ducts and out of the body.
Procedure: The patient lies on a table or water-filled cushion. High-energy shock waves are directed from outside the body onto the stones, breaking them into tiny pieces.
Benefits: Non-invasive method. May eliminate the need for surgery in select patients.
Risks: Not always effective for all stone types or sizes. There’s also a risk of the fragments causing blockages in the bile ducts.
It’s worth mentioning that while these procedures offer less invasive alternatives, they might not address the root cause of stone formation. Hence, the recurrence of gallstones remains a possibility, and ongoing monitoring is recommended. Always consult with healthcare professionals to determine the most suitable approach based on individual circumstances.
Recommended: What Emotions Affect The Gallbladder?
Treatment 3: Surgery
For many patients, especially those with recurrent symptoms or complications from gallstones, surgery is the most definitive treatment. Surgery not only addresses the immediate issue of existing gallstones but also eliminates the environment in which they form: the gallbladder itself. Here’s a comprehensive exploration of the surgical options available:
1. Laparoscopic Cholecystectomy (Keyhole Surgery)
This is the most common surgery for gallstones and involves removing the gallbladder using minimally invasive techniques.
Procedure: Small incisions are made in the abdomen. A laparoscope (a long, thin tube with high-intensity light and a high-resolution camera) is inserted, allowing the surgeon to see the area on a video screen. Surgical instruments are used to remove the gallbladder.
Benefits: Minimally invasive, which typically means shorter hospital stays, quicker recovery, and less post-operative pain. Low risk of complications.
Risks: As with all surgeries, there’s a risk of bleeding, infections, and injury to surrounding structures. There’s also a slight chance of bile duct injuries.
2. Open Cholecystectomy
This traditional method of gallbladder removal is less common nowadays but is still performed when laparoscopic methods are deemed unsuitable.
Procedure: A large incision is made in the abdomen. The gallbladder is then directly accessed and removed.
Benefits: Allows for a direct and larger access point, which can be beneficial in complex cases or when complications arise.
Risks: Compared to laparoscopic methods, there’s typically more pain, a longer recovery period, and a higher risk of complications like infections.
3. Robot-Assisted Cholecystectomy
An advanced technique that combines the minimally invasive approach of laparoscopy with the precision of robotic assistance.
Procedure: Similar to laparoscopic cholecystectomy, but the surgeon uses a robot-assisted surgical system, offering better visualization and more precise instrument control.
Benefits: Enhanced dexterity, flexibility, and control for the surgeon. Potential for even smaller incisions and quicker recovery.
Risks: As with other surgical methods, there’s a risk of bleeding, infections, and injury to surrounding structures.
Post-Surgery Considerations
- Life Without a Gallbladder: The gallbladder acts as a storage unit for bile. However, it’s not a vital organ, and the body can adapt to its absence. After its removal, bile flows directly from the liver into the small intestine. Some people might experience changes in digestion, like more frequent bowel movements or intolerance to certain foods.
- Recovery Time: Recovery from laparoscopic cholecystectomy is generally quick, with most individuals resuming normal activities within a week. Recovery from open surgery might take longer, typically ranging from 3 to 6 weeks.
- Long-term Outlook: The majority of patients find complete relief from gallstone symptoms post-surgery. However, it’s essential to maintain a balanced diet and monitor for any digestive changes.
While surgery is a significant decision, for many, it offers a permanent solution to gallstones and the discomfort and complications they can cause. Always discuss potential risks and benefits with a healthcare professional before proceeding.

Alternative and Emerging Treatments
While the treatments already outlined are the most commonly practiced and clinically accepted, the field of medicine is ever-evolving. New therapies, both alternative and scientific, are being researched and experimented with regularly.
Here’s a glance into some alternative and emerging treatments for gallstones:
Herbal and Natural Remedies
- Milk Thistle (Silymarin): Believed to stimulate the liver and bile production, it might help in decreasing the concentration of cholesterol in the bile. However, concrete evidence supporting its efficacy in gallstone treatment is limited.
- Peppermint Oil: Some studies suggest that terpene, a compound found in peppermint oil, can dissolve gallstones when taken in capsule form. However, its effectiveness and safety are still under investigation.
- Dandelion and Chicory: Traditionally believed to support liver and bile production, but scientific evidence is limited.
Note: It’s essential to consult with a healthcare professional before trying any herbal remedies, as they can interact with other medications or conditions.
Recommended: What Foods Heal The Gallbladder?
Dietary Changes and Supplements
- High-fiber diets with whole grains, fruits, and vegetables might help prevent gallstone formation.
- Reducing saturated fats and opting for unsaturated alternatives can support liver health and balance cholesterol levels.
- Vitamin C supplements might prevent gallstone formation by converting cholesterol into bile acids.
Gallbladder Flush or Cleanse
Anecdotal accounts and some alternative health practitioners advocate for “gallbladder flushes” or “liver flushes” that involve consuming a combination of olive oil, herbs, and fruit juice.
Efficacy and Safety: There is significant skepticism and a lack of scientific evidence to back these claims. Additionally, such flushes can be harmful, potentially causing nausea, vomiting, diarrhea, or abdominal pain.
Emerging Medical Therapies
- New Drug Therapies: Research is ongoing to find more effective and faster-acting medications for dissolving gallstones.
- Advanced Imaging Techniques: As technology advances, we’re seeing better imaging methods that can detect gallstones with even higher accuracy. Improved imaging can guide non-invasive treatments more effectively.
- Genetic and Molecular Research: Understanding the genetic factors that contribute to gallstone formation might open doors to preventive therapies or treatments targeting the root cause of the condition.
Bioacoustic Medicine
A relatively new field, bioacoustic medicine uses sound waves to detect irregularities in organs, including the gallbladder.
Potential Use: In the future, specific sound frequencies might be used therapeutically to break or dissolve gallstones, much like how lithotripsy works for kidney stones.
Probiotic Therapies
The gut microbiome’s role in various health conditions is a growing field of interest. Some research suggests that an imbalance in gut bacteria can influence gallstone formation.
Potential Use: Probiotic therapies might be employed in the future to balance gut flora and potentially prevent gallstone formation.
Recommended: Can Gallbladder Pain Wake You Up At Night?
In exploring alternative and emerging treatments, it’s crucial for patients to maintain a discerning attitude. While some alternative treatments might offer relief, it’s essential to rely on evidence-based practices and consult healthcare professionals before trying new or unconventional therapies.
Lifestyle Adjustments Post-Treatment
Whether an individual has undergone surgical removal of the gallbladder, minimally invasive procedures, or nonsurgical treatments, certain lifestyle adjustments can enhance recovery and reduce the risk of complications or recurrence.
Here are some recommended changes and considerations:
1. Dietary Adjustments
- Gradual Introduction of Fats: After gallbladder removal or treatment, the body may initially have difficulty digesting fats. Begin with a low-fat diet and slowly reintroduce healthy fats to monitor tolerance.
- Smaller, Frequent Meals: Consuming smaller amounts of food at regular intervals can help the liver produce a continuous, steady amount of bile, aiding digestion without overworking the system.
- Avoid Ultra-processed Foods: These foods are often high in unhealthy fats and can stress the digestive system. Opt for whole foods with minimal additives.
- Stay Hydrated: Drinking plenty of water supports overall health and digestion.
- Increase Fiber Intake: A fiber-rich diet helps regulate bowel movements and reduces the risk of constipation, which can be a concern post-surgery.
2. Physical Activity
- Gradual Resumption: Especially after surgical interventions, it’s essential to ease back into physical activities. Start with light walks and gradually intensify your exercise routine as your body heals and adjusts.
- Regular Movement: Helps in preventing constipation and supports overall health. It can also enhance mood and energy levels during the recovery phase.
3. Weight Management
- Steady Weight Loss: If advised to lose weight, aim for a gradual and steady process. Rapid weight loss can increase the risk of gallstones.
- Balanced Diet: Maintain a balanced diet that supports your nutritional needs without causing sudden weight fluctuations.
4. Medications and Supplements
- Consistent Monitoring: If you’ve been on medications like bile acid pills, ensure regular check-ups with your healthcare provider to monitor efficacy and side effects.
- Enzyme Supplements: Some people benefit from enzyme supplements that aid fat digestion post-gallbladder removal. Always consult with a healthcare professional before starting any supplement.
5. Alcohol and Caffeine Consumption
Moderation: Limit or moderate alcohol and caffeine intake, especially in the initial weeks post-treatment, to reduce stress on the digestive system.
6. Emotional Well-being
- Seek Support: Undergoing medical treatments can be emotionally taxing. It’s essential to reach out for support, be it through friends, family, or professional counseling.
- Mindfulness Practices: Activities like meditation, deep breathing exercises, and journaling can help cope with post-treatment anxieties and promote relaxation.
7. Regular Medical Check-ups
- Monitor Recovery: Regular visits to your healthcare provider will ensure that recovery is on track and that any potential complications are addressed promptly.
- Discuss Symptoms: If you experience any new or recurrent symptoms like pain, bloating, or digestive issues, discuss them with your doctor.
Recommended: Is Sugar Bad For Gallbladder?
Adjusting one’s lifestyle post-treatment is not only about healing but also about ensuring a quality of life. It’s essential to be patient with the body, recognizing that everyone’s pace of recovery is different. A proactive approach, combined with regular medical guidance, will go a long way in ensuring a smooth transition back to daily life.
Conclusion
Gallstones, while common, can profoundly impact one’s quality of life. Fortunately, a spectrum of treatments, ranging from nonsurgical methods to surgical interventions, offers effective solutions. Emerging therapies and alternative treatments also hint at a future with even more diverse options.
Regardless of the chosen treatment path, integrating lifestyle adjustments post-treatment is vital for holistic recovery and preventing potential complications. As medicine continues to evolve, staying informed and proactive in one’s health journey ensures the best outcomes. Remember, personal well-being is a blend of informed choices, timely interventions, and consistent care.
[…] Recommended: What Are The 3 Treatments For Gallstones? […]
[…] Recommended: What Are The 3 Treatments For Gallstones? […]
[…] Recommended: What Are The 3 Treatments For Gallstones? […]
[…] Recommended: What Are The 3 Treatments For Gallstones? […]